Few words in cancer care carry as much emotional weight as “recurrence.” For many patients, the fear of cancer coming back lingers long after treatment ends. When recurrence is suspected or confirmed, pathology once again becomes central to answering the most important questions. How do doctors know the cancer has returned? Is it the same cancer or a new one? What does the pathology report actually prove?
At Honest Pathology, patients frequently seek clarity around recurrence because pathology reports often feel even more confusing the second time around. Understanding how recurrence is detected and confirmed can help patients feel more grounded during an emotionally overwhelming time.
What Cancer Recurrence Means in Pathology
Cancer recurrence refers to the return of cancer after a period during which it could not be detected. From a pathology standpoint, recurrence is not based on symptoms or imaging alone. It requires direct evidence of cancer cells in a tissue or fluid sample.
Pathology confirms recurrence by identifying malignant cells that match the original cancer’s defining characteristics. This confirmation is critical because imaging findings or blood test abnormalities alone cannot definitively distinguish recurrence from scar tissue, inflammation, or treatment-related changes.
Here, accurate diagnosis plays a critical role—not just for common solid tumors but also for hematologic malignancies like leukemia where distinguishing relapse from treatment-related changes can be especially challenging.
How Pathologists Distinguish Recurrence From Treatment Effects
One of the most challenging aspects of detecting recurrence is separating true cancer from the effects of prior treatment. Surgery, radiation, chemotherapy, and immunotherapy can all alter normal tissue and create changes that appear suspicious under the microscope.
Pathologists assess cell shape, growth patterns, tissue organization, and cellular behavior to determine whether abnormal findings represent active cancer or benign post-treatment effects. Special stains, immunohistochemistry, and molecular testing are often required to make this distinction.
At Honest Pathology, patients often gain reassurance when they learn that not every abnormal finding represents recurrence and that pathologists are trained to recognize therapy-related changes.
The Role of Biopsy in Confirming Recurrence
Pathologic confirmation of recurrence usually requires a biopsy. While imaging studies may raise concern and blood tests may suggest disease activity, tissue diagnosis remains the gold standard.
A biopsy allows direct examination of cells and provides definitive evidence of malignancy. In some cases, pathologists analyze fluid samples rather than solid tissue, but the principle remains the same. Treatment decisions depend on pathologic certainty, not suspicion alone.
Especially in cancers where recurrence patterns can be unpredictable—for example, aggressive skin cancers requiring precise melanoma diagnosis—biopsy confirmation is indispensable.
Local Recurrence and Metastatic Disease in Pathology
Pathology helps determine whether recurrence is local, regional, or distant. Local recurrence occurs near the original tumor site, while metastatic recurrence involves spread to other organs or tissues.
The pathology report often compares the recurrent tumor’s features to the original cancer. Similar histology and biomarker patterns support recurrence, while significant differences may prompt consideration of a new primary cancer.
This distinction has major implications for treatment planning and prognosis.
Comparing Recurrent Cancer to the Original Tumor
When recurrence is suspected, pathologists frequently review the original pathology report and, when available, the original slides. Comparing old and new specimens helps confirm that the cancer has returned rather than representing a different disease process.
This comparison is just as critical in cancers with rapid biological changes, such as those requiring a pancreatic cancer diagnosis where initial tumor biology can influence how recurrence manifests histologically
Biomarker Changes in Recurrent Cancer
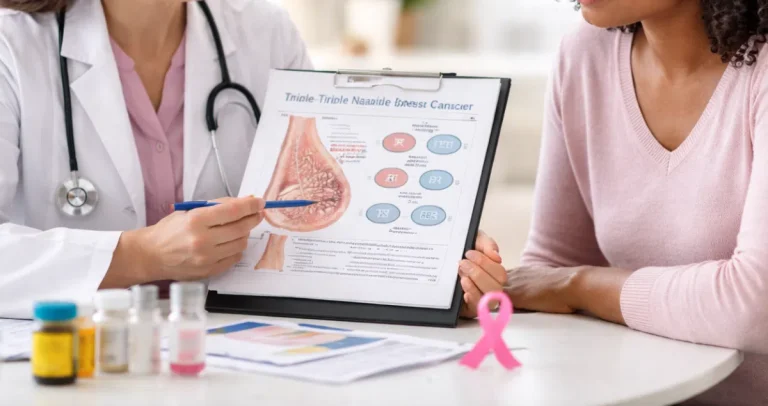
Cancer is not static. Over time and under treatment pressure, tumors can change biologically. As a result, biomarkers may differ between the original diagnosis and recurrence.
Pathology reports for recurrent disease frequently include repeat biomarker testing to guide therapy. Changes in hormone receptor status, HER2 expression, immune markers, or genetic mutations can significantly influence treatment options.
Understanding these changes helps patients and physicians make informed decisions, rather than assuming prior results still apply.
Pathology and Early Detection of Recurrence
Pathology does not screen for recurrence on its own. Instead, it confirms recurrence once suspicious findings are sampled. Surveillance strategies aim to identify changes that warrant tissue sampling before symptoms become severe.
When recurrence is confirmed early, patients may have more treatment options. Pathologic confirmation ensures that these decisions are based on evidence rather than assumption.
What “No Evidence of Disease” Means in Pathology
When a pathology report states that no cancer is identified, it means that no malignant cells were seen in the examined tissue. This is reassuring but does not guarantee that microscopic disease is absent elsewhere.
Pathology provides answers based on the tissue sampled. Honest Pathology helps patients understand both the strengths and limitations of pathology findings so reassurance is balanced with realism.
Margins, Scar Tissue, and Recurrence Evaluation
Surgical pathology reports often include margin status, which describes whether cancer cells were present at the edges of removed tissue. Margin status influences recurrence risk and how future findings are interpreted.
Scar tissue and fibrosis near prior surgical sites can complicate interpretation. Pathologists carefully evaluate these areas to determine whether changes represent healing or recurrent disease.
Understanding margin terminology can help patients contextualize later biopsies in the same region.
Timing of Recurrence and Pathologic Detection
Recurrence can occur at any point after treatment, from months to many years later. Pathology confirms recurrence whenever it occurs, regardless of timing.
The interval between treatment and recurrence reflects cancer biology rather than patient behavior or choices. Honest Pathology reinforces that recurrence is not a personal failure but a biological event.
Indeterminate and Borderline Pathology Findings
Not all pathology results provide immediate clarity. Some reports describe atypical cells, suspicious findings, or changes that require close monitoring rather than definitive treatment.
These results can be emotionally challenging. Honest Pathology helps patients interpret these findings, understand recommended next steps, and recognize when watchful waiting is appropriate.
Second Opinions in Recurrence Detection
Second pathology opinions are common when recurrence is suspected or when findings are subtle. A second review can confirm recurrence, clarify ambiguous features, or rule out malignancy.
Given the high stakes involved, obtaining additional expertise is often a prudent step rather than a sign of doubt or distrust.
Blood-Based Testing and Pathology
Blood-based tests can support monitoring but do not replace tissue diagnosis. While emerging technologies provide valuable information, pathology remains essential for confirming recurrence and guiding therapy selection.
Understanding the complementary roles of blood tests and pathology helps patients navigate evolving diagnostic strategies.
Emotional Impact of Pathologic Confirmation
Receiving confirmation of recurrence through pathology can be devastating. Patients may experience shock, grief, anger, or fear. Clear explanations do not eliminate these emotions, but they can reduce confusion and restore a sense of control.
Honest Pathology approaches these conversations with empathy, recognizing the emotional weight carried by every word in a pathology report.
How Honest Pathology Supports Patients Facing Recurrence
Honest Pathology exists to help patients understand pathology reports at every stage of cancer care, including recurrence. By translating complex findings into plain language and providing context, Honest Pathology empowers patients to engage confidently with their care team.
This clarity is especially valuable in cases like testicular cancer, where recurrence surveillance and interpretation of pathology findings are tightly linked to long-term management.
Moving Forward After Recurrence Detection
Pathology confirms recurrence, but it does not define what comes next. Many recurrent cancers are treatable, and new therapies continue to expand available options.
Understanding pathology findings allows patients to focus on next steps rather than unanswered questions. With clarity and support, patients can move forward with confidence even in uncertain circumstances.
Final Thoughts on Cancer Recurrence and Pathology
Cancer recurrence is one of the most difficult moments in a patient’s journey, and pathology sits at the center of its detection. By identifying cancer cells, distinguishing them from treatment effects, and guiding future care, pathology provides clarity when it matters most.
When patients understand how recurrence is detected and what their pathology report truly means, fear is often replaced with understanding. With support from services like Honest Pathology, pathology becomes not just a diagnostic tool, but a source of empowerment and direction during a critical moment in care.