If you’ve ever opened a cancer pathology report and felt overwhelmed by unfamiliar terms, you are not alone. Words like “biomarkers,” “mutations,” “expression,” and “amplification” can feel abstract, technical, and intimidating. Yet these terms increasingly guide some of the most important decisions in modern cancer care. Understanding what biomarkers mean in a cancer report can help patients feel more informed, empowered, and confident when discussing treatment options with their care team.
At Honest Pathology, one of the most common questions patients ask is what their biomarkers actually mean and how they affect real-world decisions. Biomarkers are not just lab jargon. They are clues about how a cancer behaves, how aggressive it may be, and which treatments are more or less likely to work.
What Is a Biomarker in Cancer?
A biomarker is a measurable biological feature that provides information about a disease. In cancer, biomarkers are usually found in tumor tissue, blood, or other bodily samples and help describe the molecular characteristics of a tumor. These characteristics go beyond what cancer looks like under a microscope and instead focus on what is happening inside the cancer cells at a genetic or protein level.
In practical terms, a biomarker can indicate whether a cancer is likely to grow quickly or slowly, whether it might respond to a specific drug, or whether certain therapies are unlikely to be effective. Biomarkers are one of the key reasons cancer treatment has shifted toward precision medicine, where therapies are increasingly tailored to the individual patient rather than applied uniformly to everyone with the same diagnosis.
How Biomarkers Appear in a Pathology Report
Biomarkers are typically reported in a dedicated section of a pathology report, often labeled as molecular testing, immunohistochemistry, genomic testing, or ancillary studies. The exact layout varies by laboratory, but the goal is the same: to summarize what specific tests were performed and what they revealed about the tumor.
Some biomarkers are reported as present or absent, while others are reported as positive or negative, overexpressed or not overexpressed, mutated or wild type. In many reports, you may also see percentages, scores, or descriptive interpretations provided by the pathologist. These details can feel confusing, especially when they are not clearly explained during a clinic visit.
This is where services like Honest Pathology can be especially helpful, translating technical findings into plain language and connecting them to real clinical implications.
Genetic Biomarkers and Mutations
One major category of cancer biomarkers involves genetic changes, also called mutations. These are alterations in the DNA of cancer cells that drive their growth and survival. Some mutations occur randomly, while others are linked to environmental exposures or inherited risk factors.
Common examples include mutations in genes such as EGFR, KRAS, BRAF, BRCA1, BRCA2, TP53, and PIK3CA. When a pathology report lists a mutation, it does not necessarily mean the mutation was inherited. Most cancer mutations are acquired and exist only in the tumor.
The presence or absence of certain mutations can directly affect treatment decisions. Some mutations predict sensitivity to targeted therapies, while others predict resistance. For patients, understanding whether a mutation is actionable is often more important than understanding the mutation itself.
Protein Expression Biomarkers
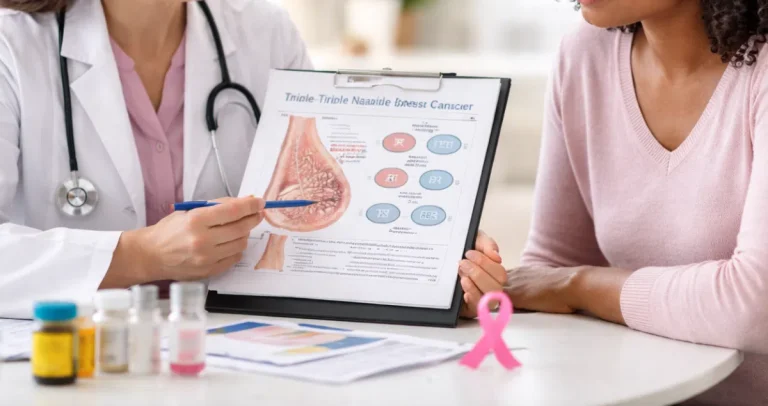
Not all biomarkers involve DNA. Many focus on proteins that are made by cancer cells. These proteins can be measured using a technique called immunohistochemistry, often abbreviated as IHC in pathology reports.
Protein expression biomarkers include well-known examples such as HER2 in breast and gastric cancers, PD-L1 in multiple tumor types, estrogen and progesterone receptors in breast cancer, and mismatch repair proteins in colorectal and endometrial cancers.
When a report describes protein expression, it may include terms like positive, negative, high expression, low expression, or a numerical score. These results help oncologists determine whether specific therapies, such as hormone therapy or immunotherapy, are appropriate.
At Honest Pathology, patients often ask why two people with the same cancer diagnosis receive very different treatments. Protein expression biomarkers are a major reason why.
Predictive vs Prognostic Biomarkers
Not all biomarkers serve the same purpose. Some are predictive, meaning they help predict whether a patient will benefit from a particular therapy. Others are prognostic, meaning they provide information about overall disease behavior regardless of treatment.
A predictive biomarker might indicate that a tumor is likely to respond to immunotherapy or a targeted drug. A prognostic biomarker might suggest whether a cancer has a higher or lower risk of recurrence.
Understanding this distinction is important because a biomarker that sounds alarming may not actually change treatment options, while a subtle finding could have major implications for therapy selection.
Biomarkers and Targeted Therapy
Targeted therapies are drugs designed to interfere with specific molecular pathways that cancer cells rely on. These therapies are often effective only when a specific biomarker is present.
For example, some lung cancers respond dramatically to drugs that target EGFR mutations, while others do not benefit at all. Similarly, HER2-positive cancers can respond to HER2-directed therapies, while HER2-negative cancers will not.
When patients see these results in their pathology report, it can feel like their future hinges on a single word. Honest Pathology helps patients understand that while biomarkers are powerful tools, they are part of a bigger clinical picture that includes stage, overall health, and treatment goals.
Biomarkers and Immunotherapy
Immunotherapy has transformed cancer treatment, but it does not work for everyone. Biomarkers play a crucial role in identifying who is most likely to benefit.
Markers such as PD-L1 expression, tumor mutational burden, and mismatch repair deficiency can suggest a higher likelihood of response to certain immunotherapies. These markers are often reported in complex ways, with percentages, cutoffs, and lab-specific interpretations.
Patients often assume that a “negative” result means immunotherapy is not an option, but that is not always true. Biomarkers guide decisions, but they do not always provide absolute answers. Honest Pathology emphasizes nuance, helping patients understand what results do and do not mean.
Why Biomarker Testing Is Sometimes Incomplete
One source of frustration for patients is discovering that not all possible biomarkers were tested. This can happen for several reasons, including limited tissue, cost considerations, or evolving standards of care.
In some cases, additional testing may be appropriate, especially if new treatments become available or if the cancer progresses. Reviewing a pathology report with an expert can help identify whether important biomarkers were not assessed and whether additional testing should be discussed with the care team.
This is one area where patients working with Honest Pathology often gain clarity and confidence in advocating for themselves.
Common Misunderstandings About Biomarkers
Many patients assume biomarkers provide certainty, but cancer biology is rarely that simple. A positive biomarker does not guarantee a treatment will work, and a negative biomarker does not always mean a treatment will fail.
Another common misunderstanding is assuming biomarkers reflect personal health choices or inherited traits. Most biomarkers reflect changes within the tumor itself and are not caused by anything a patient did or did not do.
Clear explanations can reduce unnecessary anxiety and help patients focus on what matters most: making informed decisions in partnership with their doctors.
How Pathologists Interpret Biomarkers
Pathologists play a central role in biomarker testing and interpretation. They ensure the right tests are ordered, confirm that results are technically valid, and provide context for how findings should be interpreted.
However, pathology reports are primarily written for clinicians, not patients. As a result, they often lack explanations in plain language. Honest Pathology bridges this gap by translating reports into clear, patient-friendly insights while preserving medical accuracy.
Using Biomarker Information in Shared Decision-Making
When patients understand their biomarkers, they are better equipped to participate in shared decision-making. This does not mean patients need to become molecular biologists. It means having enough understanding to ask informed questions and weigh options.
Questions such as whether a treatment is targeted to a specific biomarker, whether alternatives exist, and whether additional testing could change options become easier to ask when the report makes sense.
Biomarkers can also help patients understand why a recommended treatment may differ from what they have read online or heard from others with the same diagnosis.
The Future of Biomarkers in Cancer Care
Biomarker testing continues to evolve rapidly. New markers are being discovered, testing technologies are becoming more sensitive, and treatments are increasingly designed around specific molecular features.
As this field grows, pathology reports may become even more complex. This makes patient-centered interpretation more important than ever. Honest Pathology is built around the belief that patients deserve transparency, clarity, and respect when it comes to understanding their medical information.
Final Thoughts on Biomarkers and Empowerment
Biomarkers are not just technical details buried in a pathology report. They are powerful tools that shape modern cancer care. While they can feel intimidating at first, understanding their role can transform confusion into clarity.
By taking the time to review and explain biomarkers in plain language, services like Honest Pathology help patients move from feeling overwhelmed to feeling informed. Knowledge does not eliminate uncertainty, but it can replace fear with understanding and passivity with participation.
In a world of increasingly personalized cancer care, understanding biomarkers is no longer optional. It is a critical step toward informed, empowered, and patient-centered decision-making.