Immunohistochemistry, often abbreviated as IHC, is one of the most important yet confusing sections of a cancer pathology report. Patients commonly encounter lists of unfamiliar protein names followed by terms such as positive, negative, weak, strong, or percentages, without clear explanations of what any of it means. Despite the technical language, immunohistochemical findings often play a decisive role in confirming a diagnosis and guiding treatment.
Understanding how IHC works and how it applies to different cancer types can help patients feel more confident and informed when reviewing their pathology reports.
What Immunohistochemistry Means in Pathology
Immunohistochemistry is a laboratory technique used to detect specific proteins within cells. These proteins act as identifiers that help pathologists determine what type of cells are present and how those cells behave.
During testing, antibodies are applied to tissue samples. If the targeted protein is present, the antibody binds to it and produces a visible color change under the microscope. Pathologists then interpret the location of staining, how intense it appears, and how many cells are involved.
IHC does not replace routine microscopic evaluation. Instead, it adds a molecular layer of information that increases diagnostic accuracy and clinical relevance.
Why Immunohistochemical Findings Matter
Many cancers can appear similar under the microscope, particularly when tumors are poorly differentiated or metastatic. Immunohistochemistry helps distinguish between cancer types, confirm tissue of origin, and identify features that influence treatment selection.
For patients, this means IHC findings often explain why one treatment is recommended while another is not. These tests are not abstract or experimental; they directly affect care decisions.
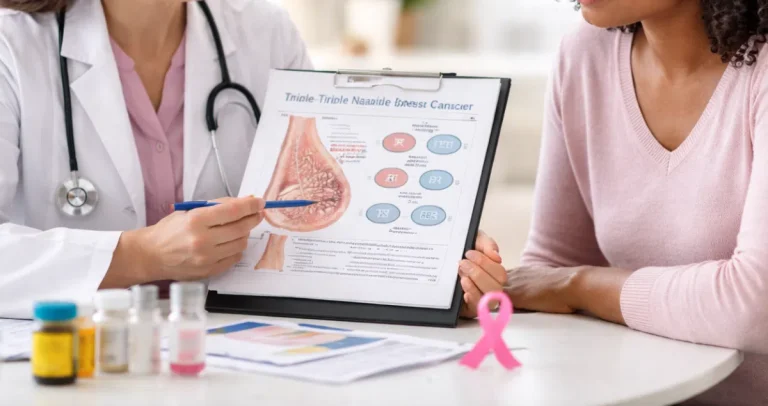
Understanding Immunohistochemistry in Breast Cancer
Breast cancer pathology reports rely heavily on immunohistochemistry because treatment is closely tied to protein expression. Estrogen receptor and progesterone receptor testing evaluates whether cancer cells depend on hormones for growth. When these receptors are present, hormone-blocking therapies may be effective.
HER2 testing assesses whether cancer cells overexpress the HER2 protein. HER2-positive cancers may respond to targeted therapies, while HER2-negative cancers will not benefit from those treatments. HER2 results are often reported using scores that reflect staining intensity and pattern.
Another commonly reported marker is Ki-67, which reflects how actively cancer cells are dividing. While it does not independently determine treatment, it provides insight into tumor behavior.
Understanding that these markers guide therapy rather than predict outcomes can help patients interpret breast cancer pathology reports more clearly.
Interpreting Hormone Receptor Results in Breast Cancer
Hormone receptor results are usually reported as positive or negative, often with a percentage of cells showing staining. Even low-level positivity may be clinically meaningful.
Patients sometimes assume that a negative hormone receptor result implies a worse prognosis, but this is not necessarily true. It simply indicates that hormone-based therapies are unlikely to be effective. Other treatment options may still be highly successful.
Understanding Immunohistochemistry in Lung Cancer
In lung cancer, immunohistochemistry is essential for distinguishing between major cancer subtypes. Stains such as TTF-1 and Napsin A support a diagnosis of lung adenocarcinoma, while p40 and p63 are associated with squamous cell carcinoma.
This distinction matters because treatment strategies differ significantly between these subtypes. Certain therapies are effective in one but not the other, and eligibility for clinical trials may depend on these findings.
IHC is also critical when a tumor is discovered outside the lungs and the origin is unclear. Staining patterns help pathologists determine whether the cancer began in the lung or spread from another organ.
Immunohistochemistry and Immunotherapy in Lung Cancer
While many lung cancer biomarkers are identified through molecular testing, immunohistochemistry plays an important role in evaluating PD-L1 expression. PD-L1 is a protein that helps predict whether immunotherapy may be beneficial.
PD-L1 results are often reported as a percentage of tumor cells staining positive. These numbers can feel arbitrary, but they are used as general guides rather than absolute rules. Treatment decisions are based on the full clinical picture, not a single value.
Understanding Immunohistochemistry in Colon Cancer
In colon cancer, immunohistochemistry is commonly used to evaluate mismatch repair proteins. These proteins help repair DNA damage. When one or more of these proteins are absent, the tumor is described as mismatch repair deficient.
Mismatch repair status influences prognosis, treatment decisions, and the need for further genetic evaluation. Pathology reports typically list whether each protein is present or absent, which can be confusing without explanation.
This testing does not diagnose inherited cancer syndromes on its own. It serves as a screening tool that may prompt additional evaluation when appropriate.
Immunohistochemistry and Treatment Implications in Colon Cancer
Mismatch repair deficient tumors may respond differently to certain therapies, including immunotherapy. Understanding this status helps explain why treatment recommendations may differ between patients with otherwise similar diagnoses.
Clear interpretation prevents patients from assuming the worst when abnormal findings are reported.
Understanding Immunohistochemistry in Prostate Cancer
In prostate cancer, immunohistochemistry is often used to confirm diagnosis, especially in small or ambiguous biopsy samples. Markers such as PSA, PSAP, and NKX3.1 help confirm that cancer originated in the prostate.
Basal cell markers are also commonly used. Their absence supports a diagnosis of cancer, while their presence suggests benign prostate tissue. These stains are diagnostic tools rather than indicators of aggressiveness or prognosis.
Immunohistochemistry in Advanced Prostate Cancer
As prostate cancer progresses or spreads, it may lose expression of traditional markers. Immunohistochemistry helps pathologists adapt to these changes and confirm diagnosis using alternative markers.
This explains why immunohistochemical findings may differ between initial diagnosis and later disease stages.
Why Immunohistochemical Results May Change Over Time
Patients sometimes notice differences in IHC results across multiple pathology reports. This can occur due to tumor evolution, treatment effects, or sampling differences.
These changes do not necessarily mean an error occurred. Cancer biology is dynamic, and pathology reflects what is present in the sampled tissue at a specific moment.
How Pathologists Interpret Immunohistochemistry
Pathologists do not simply record whether a stain is positive or negative. They assess staining location, intensity, distribution, and pattern to determine whether findings are meaningful.
This interpretive expertise is why the final diagnosis and comment sections of a pathology report are more important than raw stain results alone.
Using Immunohistochemistry to Guide Care
Immunohistochemistry helps answer practical questions about diagnosis and treatment options. It does not predict outcomes with certainty and should not be viewed in isolation.
Understanding its role helps patients engage in informed conversations without overinterpreting individual results.
Making Sense of Complex Findings
For many patients, immunohistochemical findings feel abstract and impersonal, even though they directly affect care. Translating these findings into plain language can make pathology reports feel less intimidating and more useful.
This is where services like Honest Pathology can be helpful, offering clear explanations that focus on meaning rather than jargon.
Final Thoughts on Immunohistochemistry in Cancer Pathology
Immunohistochemistry is a cornerstone of modern cancer diagnosis and treatment across breast, lung, colon, and prostate cancer. While the terminology can feel overwhelming, the purpose is straightforward: to help doctors make better, more precise decisions.
When patients understand their immunohistochemical findings, pathology reports become tools for clarity rather than sources of confusion. This is especially true in complex conditions such as lymphoma, thyroid cancer, and cervical cancer diagnosis, where IHC results play a key role in confirming disease type and guiding care.
Understanding IHC is not about mastering medical terminology. It is about knowing what the findings mean for you, your treatment options, and the path forward.