Clinical trials are often described as the engine that drives medical progress. For many patients, they also represent access to cutting-edge therapies that may not yet be widely available. Yet one of the most misunderstood aspects of clinical trial participation is how eligibility is determined. While patients often assume eligibility is based on age, diagnosis, or stage alone, pathology reports play a central and often decisive role.
At Honest Pathology, many patients are surprised to learn that their pathology report may be the single most important document in determining whether they qualify for a clinical trial. Understanding how pathology findings influence eligibility can help patients avoid missed opportunities and engage more confidently in conversations with their care team.
Why Clinical Trials Depend on Pathology
Clinical trials are designed to answer very specific scientific questions. To do this accurately, researchers must carefully define who can and cannot participate. Pathology provides the objective, biological evidence needed to ensure that participants truly have the disease or molecular features being studied.
Unlike imaging or symptoms, pathology confirms diagnosis at a cellular and molecular level. It verifies the exact cancer type, grade, and biological behavior of a tumor. Without this confirmation, trial results would be unreliable, and patient safety could be compromised.
This reliance on pathology means that even small details in a report can have a major impact on trial eligibility.
Confirming the Exact Diagnosis
One of the first eligibility requirements for nearly every cancer clinical trial is a confirmed diagnosis. This goes beyond simply naming an organ or cancer type. Pathology reports specify whether a tumor is invasive or in situ, the histologic subtype, and whether the findings meet strict diagnostic criteria.
For example, a trial designed for adenocarcinoma may exclude patients whose pathology shows squamous differentiation. Similarly, certain sarcoma or lymphoma trials require very specific subtypes that can only be identified by a trained pathologist using specialized testing.
At Honest Pathology, patients often discover that their diagnosis is more nuanced than what was initially communicated verbally. These nuances can determine whether a trial is an option or not.
Tumor Grade and Its Impact on Eligibility
Tumor grade describes how abnormal cancer cells look under the microscope and often correlates with how aggressively a tumor behaves. Many clinical trials specify eligibility based on grade because treatments may perform differently in low-grade versus high-grade disease.
A pathology report that clearly documents tumor grade helps trial investigators ensure they are studying the right patient population. If grade is missing, ambiguous, or inconsistently reported, patients may face delays or disqualification until additional review is completed.
Clarifying grading language is one of the common services provided by Honest Pathology, particularly for patients exploring trial participation.
Stage-Related Pathologic Findings
Although clinical staging often incorporates imaging and physical exams, pathologic findings contribute essential staging information. Features such as tumor size, depth of invasion, lymph node involvement, and margin status frequently appear in pathology reports and are directly tied to trial eligibility.
Some trials are limited to early-stage disease, while others require advanced or metastatic cancer. Even within the same stage, specific pathologic features may influence inclusion. A patient may believe they are eligible based on stage alone, only to learn that a pathologic detail excludes them.
Understanding how these features are defined and reported can prevent confusion and frustration.
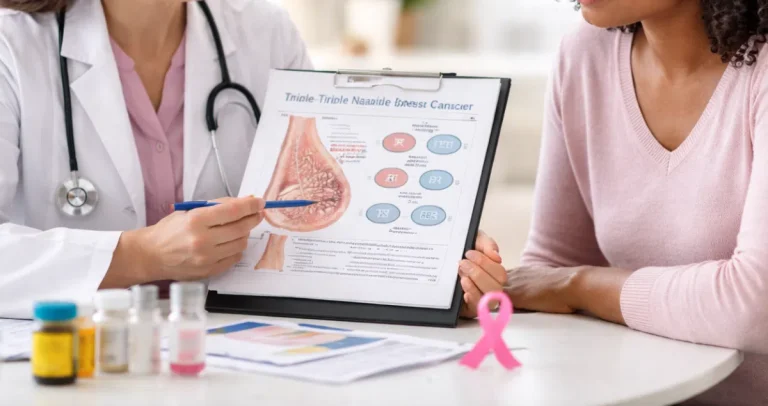
Biomarkers as Gatekeepers for Modern Trials
In modern oncology, biomarkers have become some of the most powerful gatekeepers for clinical trial eligibility. Many trials now focus on cancers with specific genetic mutations, protein expressions, or molecular signatures.
Pathology reports are where these biomarkers are documented. Molecular testing results, immunohistochemistry findings, and genomic panels often determine whether a patient can even be screened for a trial.
For example, trials investigating targeted therapies may require a specific mutation to be present. Immunotherapy trials may require certain immune markers to meet defined thresholds. Without accurate and complete biomarker reporting, patients may never be considered for these opportunities.
Honest Pathology helps patients understand which biomarkers were tested, which were not, and whether additional testing might open doors to clinical trials.
The Importance of Test Methodology
Clinical trials often specify not just which biomarker must be present, but how it must be tested. The methodology used, the type of assay, and even the laboratory performing the test can matter.
A pathology report typically documents whether a result came from immunohistochemistry, fluorescence in situ hybridization, next-generation sequencing, or another method. Trials may accept some methods and not others.
Patients are frequently unaware that a biomarker result might need to be repeated or confirmed using a different test to meet trial criteria. Honest Pathology helps decode these technical details and explains when repeat or additional testing may be worth discussing.
Tissue Adequacy and Sample Limitations
Another less visible but critical factor is tissue adequacy. Clinical trials require sufficient, well-preserved tumor tissue for eligibility confirmation and research analysis. Pathology reports often include comments about tissue quantity, quality, and limitations.
If a biopsy sample is small or degraded, it may not meet trial requirements even if the diagnosis and biomarkers are otherwise appropriate. This can be especially challenging for patients with advanced disease who have undergone multiple biopsies.
Understanding these limitations early can help patients and their physicians plan next steps, including whether a repeat biopsy is reasonable or necessary.
Exclusion Criteria Hidden in Pathology Language
Eligibility is not only about inclusion; exclusion criteria are equally important. Certain pathologic features may automatically exclude patients from specific trials due to safety concerns or scientific design.
Findings such as mixed histology, extensive necrosis, or prior treatment effects can influence eligibility. These details are often buried in descriptive sections of pathology reports and may not be immediately obvious to patients.
At Honest Pathology, reviewing reports line by line often reveals subtle exclusion factors that explain why a patient was deemed ineligible, reducing confusion and self-blame.
Central Pathology Review in Clinical Trials
Many clinical trials require a central pathology review, where an independent pathologist confirms the original diagnosis and findings. This step underscores how critical pathology is to trial integrity.
Discrepancies between local and central pathology interpretations can lead to delays or disqualification. These differences are not necessarily errors; they often reflect subjective interpretation or evolving diagnostic criteria.
Preparing patients for this possibility and helping them understand what central review means is another way Honest Pathology supports informed participation.
Timing and Pathology in Trial Enrollment
Pathology timing also affects eligibility. Some trials require recent tissue samples, while others allow archival specimens. Pathology reports document when tissue was obtained and whether it reflects current disease status.
If a report is outdated or does not represent the current biology of the cancer, a patient may need new testing. Understanding these requirements ahead of time can prevent last-minute surprises during the screening process.
Pathology Reports as Advocacy Tools
For patients seeking clinical trials, pathology reports are not just medical records; they are advocacy tools. A well-understood report allows patients to communicate clearly with oncologists, trial coordinators, and research teams.
When patients understand their pathology findings, they can ask more precise questions about eligibility and potential next steps. Honest Pathology empowers patients by transforming complex reports into actionable knowledge.
The Emotional Impact of Eligibility Decisions
Being told you are not eligible for a clinical trial can be emotionally devastating. Patients may feel rejected, confused, or hopeless, especially if they do not understand the reason.
Clear explanations rooted in pathology can help patients process these decisions more constructively. Knowing that ineligibility is based on specific biological criteria, not personal failure, can ease emotional distress and help patients explore alternative options.
How Honest Pathology Supports Trial Exploration
Honest Pathology exists to bridge the gap between complex pathology reports and patient understanding. By reviewing reports with patients, explaining findings in plain language, and highlighting factors relevant to clinical trials, Honest Pathology helps patients navigate a challenging landscape with greater confidence.
This support is particularly valuable for patients considering second opinions, additional testing, or self-directed trial searches.
Looking Ahead to Precision Trial Design
As clinical trials become more precise and biomarker-driven, the role of pathology will only grow. Future trials are likely to rely even more heavily on molecular and genetic features documented in pathology reports.
This makes patient education and transparency essential. Understanding pathology is no longer optional for patients exploring advanced treatment options.
Final Thoughts on Pathology and Trial Eligibility
Pathology reports quietly shape who gets access to clinical trials, often behind the scenes. They confirm diagnoses, define tumor behavior, identify biomarkers, and enforce eligibility criteria with scientific rigor.
By understanding how pathology influences these decisions, patients can move from feeling powerless to feeling informed. With guidance from services like Honest Pathology, pathology reports become less of a barrier and more of a roadmap.
Clinical trials offer hope, but pathology determines the path. When patients understand that path, they are better equipped to navigate it with clarity, confidence, and purpose.