Being told that a biopsy is “negative” often brings immediate relief. For many people, it feels like the end of a frightening chapter. Yet a lingering question sometimes remains, quietly or urgently: can a biopsy miss cancer? The short answer is yes, it can. The longer answer is more nuanced, and understanding it can help patients and clinicians make sense of uncertainty without losing trust in the diagnostic process.
Biopsies are powerful tools, but they are not perfect. Knowing their limitations is not a reason for fear. It is a path toward informed care.
What a Biopsy Actually Samples
A biopsy examines a small piece of tissue taken from a much larger organ or lesion. It represents a snapshot, not the entire picture. Even when performed carefully and with imaging guidance, a biopsy can only sample what the needle or instrument reaches.
Cancer is not always evenly distributed. Some tumors are heterogeneous, with malignant areas next to benign or inflamed tissue. If the sampled area does not contain cancer cells, the biopsy may return a negative result even when cancer is present elsewhere.
Why Biopsies Are Still So Valuable
Despite their limitations, biopsies remain the gold standard for diagnosing many cancers. They provide direct microscopic evidence, allowing pathologists to assess cellular detail, tissue architecture, and molecular features.
Most biopsies are accurate. When they miss cancer, it is not because the process is careless, but because biology and anatomy can be complex. Understanding this balance is key to interpreting results realistically.
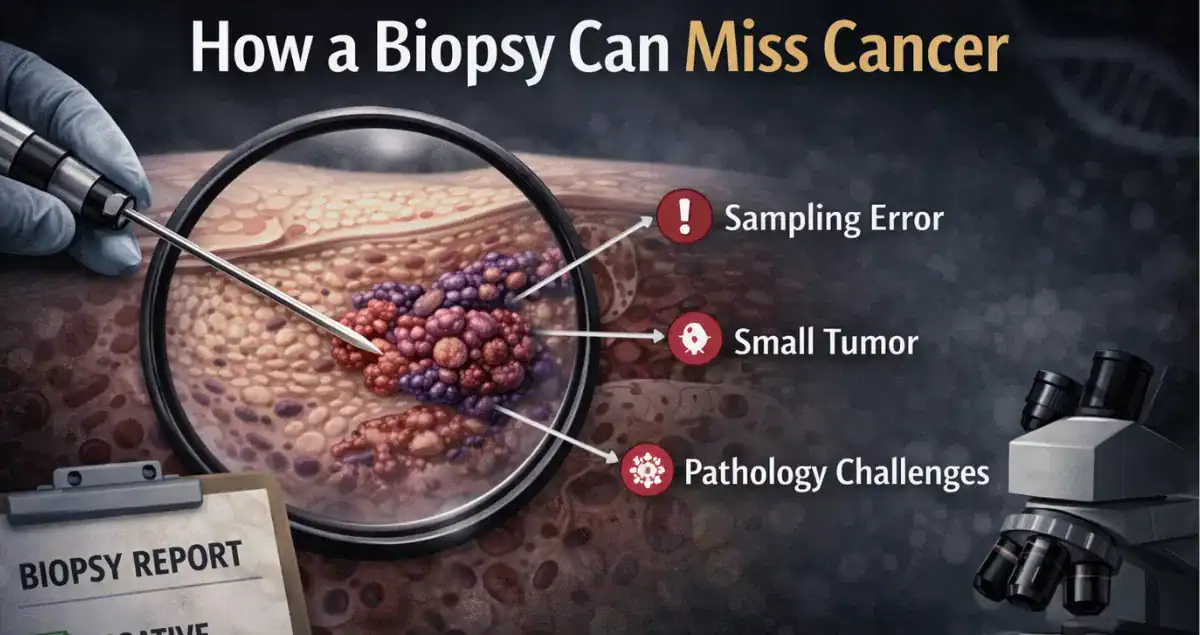 How a Biopsy Can Miss Cancer
How a Biopsy Can Miss Cancer
One common reason a biopsy may miss cancer is sampling error. The needle or forceps may simply not capture the malignant portion of a lesion. This is more likely when lesions are small, irregular, difficult to visualize, or located in hard-to-reach areas.
Another factor is tumor heterogeneity. Some cancers contain areas that appear relatively normal under the microscope, especially early in their development. Inflammatory or reactive changes can also mask subtle malignancy.
Technical factors matter as well. Tissue may be crushed, fragmented, or insufficient for full evaluation. In some cases, the amount of tissue is adequate to say what is present, but not enough to confidently exclude what is absent.
The Role of Imaging and Clinical Correlation
Biopsy results do not exist in isolation. Radiologic findings, endoscopic appearance, physical exam, and clinical symptoms all provide context. When a biopsy result does not align with imaging or clinical suspicion, that discrepancy matters.
A negative biopsy in the setting of a highly suspicious lesion is not always the end of the investigation. Repeat biopsy, additional sampling, or surgical excision may be appropriate. Medicine advances by correlating data, not by relying on a single test.
False-Negative Biopsy Results
When a biopsy fails to detect cancer that is actually present, it is referred to as a false-negative result. False negatives can be emotionally challenging because they often delay diagnosis rather than causing immediate alarm.
Importantly, false negatives are usually discovered not because someone ignored symptoms, but because ongoing follow-up raised questions. Persistent symptoms, interval growth on imaging, or new findings often prompt re-evaluation.
Why Early Cancers Are Harder to Detect
Early cancers may be small, subtle, or confined to surface layers. Architectural distortion and nuclear changes may be minimal. Distinguishing early malignancy from reactive or benign processes can be difficult, especially in limited samples.
In some organs, early cancer may be patchy or flat rather than forming a discrete mass. In these situations, even multiple biopsies can miss the lesion if sampling is not targeted precisely.
The Importance of Adequate Sampling
The number and quality of biopsy samples matter. Multiple cores or targeted biopsies increase the likelihood of capturing diagnostic tissue. In endoscopic procedures, taking multiple samples from suspicious areas improves detection rates.
Pathologists also rely on adequate tissue preservation. Poor fixation or excessive artifact can limit interpretation and increase uncertainty.
When a Negative Biopsy Is Reassuring
Not every negative biopsy is cause for concern. When clinical findings, imaging, and pathology all align, a negative result can be highly reassuring. In these cases, the likelihood of missed cancer is low.
The key is concordance. When all pieces of the puzzle point in the same direction, confidence increases.
When to Question a Negative Biopsy
A negative biopsy deserves further discussion when symptoms persist, imaging remains concerning, or clinical suspicion is high. Questioning a result does not mean distrusting the pathology. It means recognizing the limits of sampling.
Repeat biopsy or alternative diagnostic approaches are sometimes the safest next steps.
How Pathology Reports Address Uncertainty
Pathology reports often include language such as “no malignancy identified” rather than “cancer ruled out.” This wording is intentional. It reflects what was seen in the tissue examined, not a guarantee about unsampled areas.
Understanding this distinction can help patients interpret reports more accurately and avoid false reassurance.
The Emotional Impact of Uncertainty
Living with uncertainty is one of the hardest parts of medicine. A negative biopsy followed by continued symptoms can feel confusing or invalidating. Clear communication about limitations and next steps is essential for patient trust.
Uncertainty does not mean inaction. It means observation, correlation, and, when necessary, reassessment.
Why Follow-Up Matters
Follow-up is the safeguard against missed diagnoses. Surveillance imaging, repeat exams, and open communication ensure that changes are detected over time. Many cancers that are initially missed are caught later through careful follow-up, often still at a treatable stage.
Conclusion
Yes, a biopsy can miss cancer. That reality reflects the complexity of human biology, not a failure of medicine. Biopsies are powerful tools, but they work best when interpreted in context and followed thoughtfully.
Understanding the limitations of biopsy helps patients and clinicians make better decisions, ask better questions, and maintain trust in the diagnostic process.
If you have ongoing concerns about a biopsy result or want help understanding whether further evaluation is appropriate, Honest Pathology offers educational support and second-opinion pathology review recommendations focused on clarity and transparency.