Lung cancer can sound like one of the scariest diagnoses anyone can face , but understanding how lung cancer is diagnosed can help take away some of the fear. Knowing what doctors look for, what tests are done, and how the results are interpreted gives you more control and confidence during an uncertain time.
At Honest Pathology™, our mission is to help you understand your pathology report and every step of the diagnostic process in plain, easy-to-understand language. Let’s walk through how doctors, radiologists, and pathologists work together to diagnose lung cancer , from the first scan to the final report.
It All Starts With a Suspicion
Most people don’t start out thinking they have lung cancer. Instead, something triggers concern , maybe a persistent cough, shortness of breath, chest pain, or an abnormal imaging test.
In many cases, lung cancer is first suspected after a chest X-ray or CT scan shows a “spot” or “mass” in the lung. These can look like shadows or lumps on the image.
However, not every spot is cancer. Infections, inflammation, or even old scarring can cause similar changes. That’s why additional testing is essential , imaging alone cannot confirm cancer. The next step is to find out exactly what the cells are.
Imaging Tests: The First Clues
When a doctor sees something abnormal on an X-ray, the next step is usually a CT scan. A CT scan provides detailed, three-dimensional images of the lungs, showing the size and shape of a nodule or mass, whether it is solid or partially solid, if there are enlarged lymph nodes nearby, and whether it has spread, which is called metastasis.
Sometimes, doctors also order a PET scan to detect whether the abnormal area is active or growing, based on how much glucose (sugar) it absorbs, since cancer cells tend to use more sugar and therefore “light up” on the scan. These imaging tests help doctors determine the best place to take a sample for biopsy, which is key to making an accurate diagnosis.
The Biopsy: Getting a Sample of the Cells
To confirm whether a suspicious area is lung cancer, a biopsy is required. A biopsy means removing a small piece of tissue or fluid from the abnormal area to examine it under a microscope.
There are several ways a biopsy can be done, depending on the location of the abnormality:
• CT-Guided Needle Biopsy
A radiologist uses CT imaging to guide a thin needle into the lung nodule to remove a tissue sample. This is one of the most common ways to get a diagnosis.
• Bronchoscopy
A lung specialist (pulmonologist) inserts a thin, flexible tube with a camera (bronchoscope) through the mouth or nose and down into the lungs. Small tools can be passed through the tube to collect tissue samples.
• Endobronchial Ultrasound (EBUS)
This is a special type of bronchoscopy that uses ultrasound to look at and sample lymph nodes around the lungs and airways. It helps determine if cancer has spread.
• Thoracentesis
If there’s fluid around the lungs (called a pleural effusion), a doctor can remove some of it with a needle. The fluid is sent to the lab to check for cancer cells.
• Surgical Biopsy
If the other methods don’t give enough information, a surgeon may perform a small operation (called VATS, or video-assisted thoracoscopic surgery) to remove a piece of the lung for testing.
The Pathologist’s Role: Looking at Cells Under the Microscope
Once the tissue sample is collected, it goes to the pathology lab, where a pathologist , a medical doctor who specializes in diagnosing disease under the microscope , studies it carefully.
This is one of the most important steps in diagnosing lung cancer. The pathologist looks at the cells’ shape, size, and arrangement to determine whether they’re normal or malignant (cancerous).
If cancer is found, the pathologist identifies the type of lung cancer. The two main categories are:
• Non-Small Cell Lung Cancer (NSCLC)
This makes up about 85% of all lung cancers. It includes:
- Adenocarcinoma – often found in people who used to smoke or never smoked. It tends to grow in the outer parts of the lungs.
- Squamous Cell Carcinoma – linked to smoking, usually grows near the central airways.
- Large Cell Carcinoma – a less common type that can appear anywhere in the lung.
• Small Cell Lung Cancer (SCLC)
This type makes up about 15% of cases and tends to grow and spread quickly. It is usually found in people with a history of smoking.
The pathologist may also perform special stains and immunohistochemistry tests to confirm the diagnosis. These tests help identify the proteins and markers that make certain cancer cells unique.
Molecular and Genetic Testing
After a diagnosis of lung cancer is confirmed, additional molecular testing may be done on the biopsy tissue. These tests look for genetic mutations or biomarkers that can help guide treatment.
For example, in non-small cell lung cancer, your pathologist may look for mutations in:
- EGFR
- ALK
- ROS1
- KRAS
- BRAF
- PD-L1
If any of these are present, it can make a huge difference in how doctors treat your cancer. Some of these mutations respond very well to targeted therapy , pills that attack specific molecules inside the cancer cells , rather than traditional chemotherapy.
At Honest Pathology™, we often help patients understand what these results mean. When you see terms like EGFR mutation positive or PD-L1 60%, it can sound overwhelming , but each of these details provides valuable clues that can lead to more personalized treatment options.
Cytology: Diagnosing Cancer from Fluids or Brushings
Sometimes, instead of a solid tissue biopsy, the sample might come from cytology, which involves looking at individual cells rather than a piece of tissue.
Examples include:
- Sputum cytology: Examining mucus coughed up from the lungs
- Bronchial brushing/washing: Cells collected during bronchoscopy
- Pleural fluid cytology: Cells floating in fluid around the lungs
Cytology can confirm cancer in cases where a traditional biopsy isn’t possible or when fluid builds up due to cancer. The pathologist can often identify the cancer type from these cells alone.
Staging the Cancer: How Far Has It Spread?
Once the pathologist confirms cancer, the next question is how advanced it is. This is called staging.
Staging helps doctors plan treatment and predict outcomes. The most common system used is called TNM staging:
- T (Tumor): How big is the tumor, and where is it located?
- N (Nodes): Has the cancer spread to nearby lymph nodes?
- M (Metastasis): Has it spread to other parts of the body (like the brain, bones, or liver)?
Imaging tests such as CT, PET, MRI, or bone scans may be used to help determine the stage. Sometimes, pathologists also examine lymph nodes removed during surgery to finalize the staging.
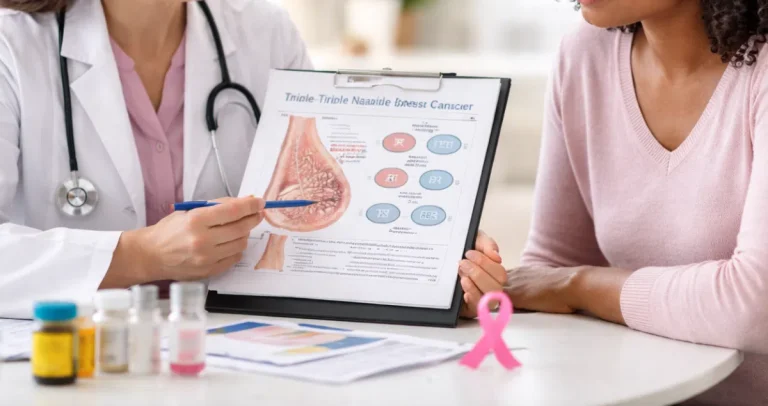
Understanding Your Pathology Report
Your pathology report is the final written document that summarizes everything the pathologist found in your biopsy. It includes several important sections:
- Diagnosis: The exact type of lung cancer
- Histologic grade: How abnormal the cells look (this can suggest how fast they may grow)
- Margins: Whether the cancer was fully removed (if surgery was done)
- Lymph node status: Whether nearby nodes show cancer cells
- Molecular findings: Any genetic or biomarker results
This report can be complex and filled with medical terms like “moderately differentiated adenocarcinoma” or “PD-L1 expression 60%.”
That’s where Honest Pathology™ can help. We translate these technical findings into clear, understandable language. Our U.S.-trained pathologists can walk you through your report line by line , so you know exactly what it means and what questions to ask your care team.
Why Early Diagnosis Matters
Catching lung cancer early can dramatically improve treatment options and survival rates. In early stages, it may be curable with surgery or radiation. Once it spreads, treatment focuses more on control and quality of life.
If you’re at risk , especially if you have a smoking history or chronic exposure to secondhand smoke , ask your doctor about low-dose CT screening. This annual scan can detect lung cancer before symptoms appear and has been shown to save lives.
Emotional Impact and Support
Being told you might have lung cancer is emotionally overwhelming. Waiting for test results can be stressful. It’s normal to feel anxious, scared, or confused by all the medical terms and tests.
During this time, knowledge truly is power. Understanding what’s happening , and why each test is necessary , can give you a greater sense of control.
At Honest Pathology™, we believe no patient should ever feel lost or alone in their diagnosis. Our consultations are designed to help you make sense of your pathology report in simple, non-technical language, so you can have informed conversations with your doctor.
Questions to Ask Your Doctor or Pathologist
When you meet with your care team, here are some helpful questions to consider:
- What type of lung cancer do I have?
- What stage is it, and what does that mean for me?
- Were any genetic mutations or biomarkers found?
- What treatments are recommended for my type and stage?
- Should I get a second opinion on my pathology report?
- Can Honest Pathology™ help me understand my results more clearly?
These questions can guide your discussion and ensure you fully understand your diagnosis and treatment plan.
Empowering Yourself With Knowledge
Lung cancer diagnosis is not a single event , it’s a process that involves multiple specialists, technologies, and steps. From imaging to biopsy to pathology, every piece of information builds a clearer picture.
Even though the terms and tests can feel complicated, you have the right to understand every part of your diagnosis. Knowledge helps you make informed choices about your treatment and gives you confidence moving forward.
That’s exactly why Honest Pathology™ exists. We’re here to bridge the gap between complex medical language and human understanding , empowering you to take an active role in your care.
Final Thoughts
The diagnosis of lung cancer involves teamwork between radiologists, pulmonologists, surgeons, and most importantly, pathologists , the doctors who confirm whether cancer is present by examining your tissue under the microscope.
If you’ve recently received a lung biopsy report or are waiting for results, know that it’s okay to ask for help understanding it. Your pathology report holds the answers to what’s going on inside your body , and Honest Pathology™ can help you make sense of every detail.
At Honest Pathology™, our mission is simple
To help patients truly understand their diagnosis , not in medical jargon, but in words that make sense. If you or a loved one has a lung biopsy or pathology report, visit www.HonestPathology.com to schedule an online educational consultation. Together, we’ll review your results step by step , so you can move forward with clarity, confidence, and peace of mind.